
Faculties Failure?
Margaret Williams
25th May 2008
There can be few in the international ME/CFS
community, either researchers or sufferers, who are
not profoundly dismayed at yet another article
co-authored by Professor Simon Wessely that fails to
distinguish between patients with chronic fatigue
and those with chronic fatigue syndrome.
His article Physical or Psychological a comparative
study of causal attribution for chronic fatigue in
Brazilian and British primary care patients (Acta
Psychiatr Scand May 2008:
doi:10.111/j.1600-0447.2008.01200.x) fails to
distinguish between chronic fatigue and chronic
fatigue syndrome, the latter also being referred to as
myalgic encephalomyelitis.
For peer-reviewers of a highly-rated journal such as
Acta Psychiatrica Scandinavica (which has an impact
factor of 3.857, this being a high score, since 90% of
journals score less than 1 on impact rating) to have
allowed such blatant misrepresentation to have
escaped censure is alarming.
It is a matter of record that when serious errors and
misrepresentations in his published articles (which,
when challenged, even Wessely himself cannot
rationally condone) have been pointed out to him
and to Editors, Wessely blames his peer-reviewers.
One instance of this occurred in 1997 in relation to
his article in the Quarterly Journal of Medicine (The
prognosis of chronic fatigue and chronic fatigue
syndrome: a systematic review. Joyce J, Hotopf M,
Wessely S. Q J Med 1997:90:223-233), the many
flaws of which were exposed by Dr Terry Hedrick (a
research methodologist) in a bullet-proof analysis
that was published in Q J Med 1997:90:723-725.
To quote Hedrick: Patients beliefs in organic bases for
their illnesses may be more accurate than anything
else we have to offer at this time. Not only did the
Joyce et al article fail to summarize the psychiatric
literature accurately, it omitted discussion of the
many avenues now being explored on the organic
underpinnings of (ME)CFS.
This is not an isolated example of Wessely blaming
his peer-reviewers.
There have been others, for example, when UK medical statistician Professor
Martin Bland from St Georges Hospital Medical
School, London, pointed out significant statistical
errors in a paper by Wessely and Trudie Chalder,
saying that Wesselys findings were clearly
impossible, Wessely absolved himself from any
blame.
Bland was robust: Potentially incorrect conclusions,
based on faulty analysis, should not be allowed to
remain in the literature to be cited uncritically by
others (Fatigue and psychological distress. BMJ: 19th
February 2000:320:515-516). Wessely was compelled
to acknowledge on published record that his figures
were incorrect: We have been attacked by gremlins.
We find it hard to believe that the usually infallible
statistical reviewers at the BMJ could have
overlooked this and wonder, totally ungallantly, if we
can transfer the blame to the production side.
Will Wessely once again try to blame his
peer-reviewers for this latest confusion and absolve
himself from any blame? By what mental mechanism
does he continue to dissociate himself from the fact
that his personal belief that ME/CFS is a behavioural
disorder is unsupported by hard evidence? Is he
unmoved by the body of irrefutable evidence that has
shown him to be wrong? That body of evidence is not
going to go away. Why does he continue to deny it?
How often must it be pointed out that it was in 1990
that the American Medical Association made it plain
that chronic fatigue and chronic fatigue syndrome are
not the same? The AMA statement said: A news
release in the July 4 packet confused chronic fatigue
with chronic fatigue syndrome; the two are not the
same. We regret the error and any confusion it may
have caused.
And yet --- eighteen years later --- here we have
Wessely and his co-authors still using the terms
chronic fatigue and chronic fatigue syndrome and
myalgic encephalomyelitis synonymously.
Does this not amount to scientific misconduct?
The title and the abstract of his latest paper refer to
chronic fatigue but the text refers to chronic fatigue
syndrome and ME.
Given the fact that chronic fatigue is not synonymous
with ME/CFS, the authors cannot possibly be talking
about patients with ME/CFS, yet they claim to be
doing so: Chronic fatigue syndrome (CFS),
sometimes also known as myalgic encephalomyelitis
(ME)..
Once again, this is in rank defiance of the World
Health Organisations International Classification of
Diseases (ICD-10, 1992), which classifies fatigue
quite separately from ME/CFS; moreover, the WHO
has provided written clarification that it is not
permitted for the same disorder to be classified to
more than one rubric. Fatigue is classified as a
mental disorder whilst ME/CFS is classified as a
neurological disorder.
Why is Wessely continually permitted to defy such
international taxonomic principles?
Unsurprisingly, this latest paper is replete with
self-references.
In it, Wessely states emphatically: British primary
care patients with unexplained chronic fatigue were
more likely to attribute their fatigue to physical
causes than their Brazilian counterparts.
Wessely acknowledges that: The study participants
were not randomly selected representative samples
from the healthcare seeking population yet his
conclusion is categoric: Causal attribution influences
symptom experience, help-seeking behaviour and
prognosis in chronic fatigue syndrome.
Wessely states: Less explored is a possible variation
in causal attribution between sociocultural settings
and to what extent physical attribution consistently
associated with a poor prognosis of CFS is enhanced
by sociocultural variables more frequently observed
in Western affluent countries such as the UK. These
include the sociopolitical debate about the
nosological status of CFS in general and for disability
benefits in particular.
Somewhat unexpectedly, Wessely concedes that CFS
is officially endorsed as a medical condition in the
UK, citing A report of the CFS/ME working group:
report to the Chief Medical Officer of an independent
working group. Hutchinson A. cited 2007 September
23 (i.e. the Report to the CMO). This is notable,
given that the original report of 11th January 2002
specifically omitted to accept the WHO classification
of ME/CFS as a neurological disorder.
If Wessely concedes that CFS is officially endorsed
as a medical condition in the UK, why does he refer
to it as unexplained chronic fatigue (UCF), which is a
WHO classified mental disorder?
It is a straight-forward enough concept, so once
again it has to be asked what is it about this
concept that Wessely seems so continually unable
or unwilling to understand?
In this latest paper, patients in the study with
unexplained chronic fatigue were identified using the
Chalder Fatigue Questionnaire, which is said to
identify substantial chronic fatigue lasting six
months or more. How this matches the criteria for
ME/CFS such as the 2003 Canadian definition by
Carruthers et al is not explained. The authors state:
The questionnaires were read out to illiterate (Brazillian) participants. Those who fulfilled criteria
for CFS were then asked to answer questions on
causal attribution, duration of fatigue, and the
Centre for Disease Control and Prevention (CDC)
1994 case definition of CFS.
Furthermore, the authors state that they relied upon
an estimated prevalence of chronic fatigue and on an
assumed prevalence of UCF.
Despite a study cohort that seems to be a
conglomeration of ill-defined participants, Wessely
et al state: More widespread awareness of CFS/ME in
the UK may lead to a greater likelihood of British
patients viewing their fatigue via a biomedical
perspective than their counterparts in Brazil. In the
UK, most media and self-help material provided by
patient organisations are more likely to promote
physical rather than psychological explanations (and)
the health care system, which labels fatigue as a
medical condition, may further reinforce this
tendency.
No reference is provided to support the assertion
that the UK health care system labels fatigue as a
medical condition.
The authors state: Social support provided in a way
which fosters dependency can help maintain chronic
fatigue (and) there is an association between
secondary gain and health outcomes (in) functional
somatic syndromes.
Wessely et al supply no references to support their
claim, and seem to ignore the fact that both the
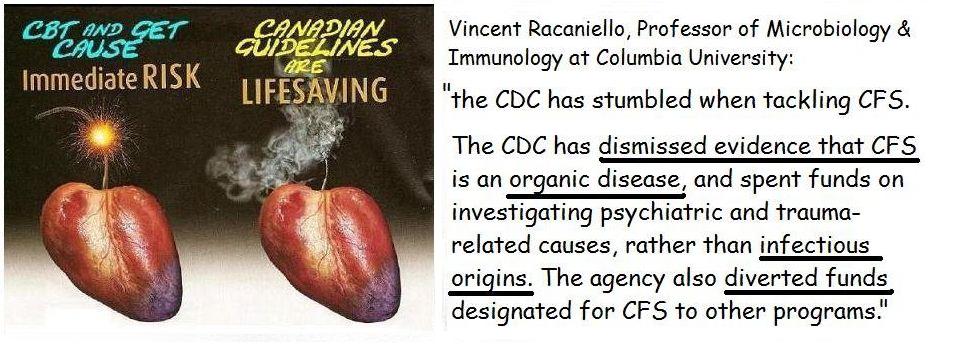
Canadian and Australian guidelines reject such a
notion.
Despite Wesselys acknowledgement that there was a
high non-response rate in the UK (Approximately
30% of the eligible patients in the UK did not
complete phase 2 in comparison with only 6% in
Brazil), the conclusion is that:
The higher availability of sick leave / sickness benefit because of CFS in the
UK may both contribute to and reflect the greater
legitimsiation of chronic fatigue as a medical
disorder. The findings of this study lend some
support to the evidence on the important role of
sociocultural factors in shaping illness attribution
and perception around chronic fatigue and chronic
fatigue syndrome.
It cannot be emphasised enough that unexplained
chronic fatigue is not the same as ME/CFS.
At the Second World Congress on CFS and related
disorders held in September 1999 in Brussels, Dr
Daniel Peterson from the US said that ten years ago
(i.e. in 1989), he believed that (ME)CFS would be
resolved by science, but that he had now changed
his mind and believed that it could only be resolved
by politics.
It is politicians whom Wessely advises on CFS/ME
and it is politicians who implement his advice,
without seeming either to be aware of or to care
about the enormous body of scientific evidence
demonstrating that Wessely is simply wrong to lump
chronic fatigue with ME/CFS as a single entity.
Can it be right that politicians should now control the
science of medicine?
Wessely seems to think so. His latest paper seems
to be saying that if Social Security benefits are
stopped, patients will stop having ME/CFS.
This contradicts the NICE Guideline on CFS/ME that
was published in August 2007, which clearly said
that it was the doctors job to support CFS/ME
patients in obtaining benefits.
It seems that Wessely disagrees.
No, it seems that he just wants his name in a paper again and again, and if you keep on telling the same story people will start to believe it and see him as the big know it all, delusional psychiatry at its best.
Also called repetitive strain psychiatry ...

1 comment:
Great post, Dr. Speedy. Just sorry it needed writing.....
Post a Comment